Summary of your benefits.
The chart below includes an overview of CareOregon Dental plan benefits. These benefits, and any other information you need, is found in your handbook. Click here for the Health Share Member Handbook or the Columbia Pacific CCO Member Handbook.
Dental benefits | Authorization/Referral? | Limits to Care? |
| Exams, cleanings, X-rays* | No authorization/referral required | At least one exam and cleaning every 12 months for adults. Two exams and cleanings every 12 months for members under 19. |
| Basic restorative care (fillings) | No authorization/referral required | No limit |
| Dentures and partials | No authorization. Referral is subject to review. | Only available for qualifying members or incidents. Call our customer service for more details. |
| Sealants* | No authorization/referral required | Every five years for children 15 and under with permanent molars. |
| Stainless steel crowns* | No authorization/referral required | Approval based on OHP guidelines. Call our customer service for more details. |
| Extraction (removing teeth) of wisdom teeth | No authorization. Referral is subject to review. | No limit |
| Orthodontics (braces) and extractions (removing teeth) for braces | Yes, authorization/referral is required | Approval based on OHP guidelines. |
| Urgent or immediate dental treatment (emergency) | No authorization/referral required | No limit |
| Orthodontics (including braces) | Preapproval is needed | For members under 21 |
*Restrictions may apply and/or preapproval may be required. A star (*) in the benefit charts means a service may be covered beyond the limits listed for members under 21, if medically necessary and appropriate.
If you have questions regarding your CareOregon Dental plan, call CareOregon Dental Customer Service at 503-416-1444, toll-free 888-440-9912
or TTY 711.
Benefits topics
Click on a topic below to expand more information.
Contact Oregon Health Authority:
- For information about enrollment, including renewals, your application status, changing your CCO and name/address changes.
The Oregon Health Authority (OHA) runs the Medicaid program for the entire state of Oregon, which is called the Oregon Health Plan (OHP).
Online: one.oregon.gov
Phone: Toll-free 800-699-9075 or TTY 711, 8 a.m. to 5 p.m. Monday-Friday
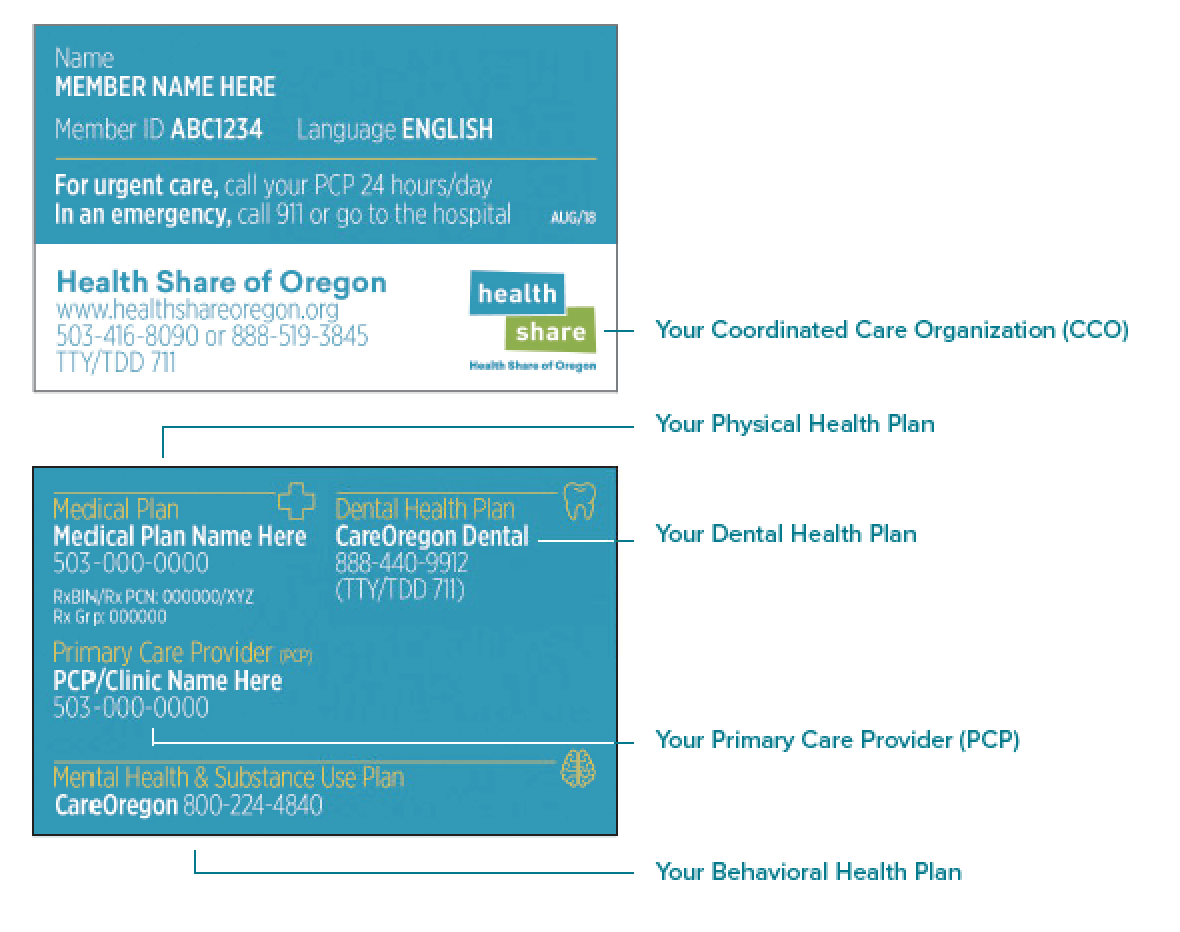
Contact Health Share of Oregon:
- To replace a lost or stolen Member ID card.
- To make a health plan or dental plan change within Health Share.
Health Share is a coordinated care organization (CCO). It’s one of two CCOs that work under OHA to serve OHP members in the tri-county area.
Online: healthshareoregon.org
Phone: 503-416-8090, toll-free 888-519-3845 or TTY 711, 8 a.m. to 5 p.m. Monday-Friday
Email: info@healthshareoregon.org
Contact CareOregon:
- To change your PCP or find a provider.
- For questions about your benefits and eligibility, such as:
- Is my coverage active?
- What medications or services are covered?
- What’s the status of my appeal or prior authorization?
- For help navigating a question or problem, or want to submit a complaint.
CareOregon is one of several insurance providers in the tri-county area that helps Health Share deliver care to OHP members.
Phone: 503-416-4100, toll-free 800-224-4840, TTY 711, 8 a.m. to 5 p.m. Monday-Friday
Email: customerservice@careoregon.org
Secure message: careoregon.org/portal
CareOregon takes fraud, waste and abuse very seriously. If you suspect that your benefits aren't being used correctly or want to report a case of fraud, waste or abuse, please contact EthicsPoint at 888-331-6524. You also can file a report online at EthicsPoint.
How to make a complaint or grievance
If you are unhappy with CareOregon or Health Share of Oregon, your health care services or your provider, you can complain or file a grievance at any time, for anything other than a denial of service. Your provider or authorized representative may also file a grievance on your behalf with your written consent.
We will try to make things better. Just call Customer Service t 503-416-1460 or toll-free at 888-519-3845, or send us a letter to the address on page 73 of your member handbook, available on the Health Share of Oregon website.
You can also fill out a complaint and feedback form here:
CareOregon and Health Share of Oregon will work to resolve your complaint or grievance as quickly as your health condition requires. If we need more than five business days, we will send you a letter to let you know why. You will receive a final answer within 30 calendar days. We will not tell anyone about your complaint unless you ask us to.
You can also file a complaint with:
Oregon Health Authority (OHA)
Please call the OHP Client Services unit (CSU) toll free at 800-273-0557 or OHA’s Ombudsman at 503-947-2346 or toll free at 877-642-0450.
Appeals and hearings
If we deny, stop or reduce a medical service your provider has ordered, we will mail you a Notice of Action letter explaining why we made that decision. You have a right to ask to change it through an appeal and a state fair hearing. You must ask for an appeal no more than 60 days from the date on the Notice of Action letter. You can ask for a denial notice that shows a service is not covered if:
- You did not receive a written notice of denial, or;
- Your provider tells you that you will need to pay for a service that is not covered.
For full instructions on the appeals process, please see page 71 of your member handbook, available on the Health Share of Oregon website.
Provider Appeals
Your provider has a right to appeal for you when their physician’s orders are denied by a plan. You must agree to this in writing. Instructions for this process can be found on page 72 of your member handbook, available on the Health Share of Oregon website.
Download one of the forms below to manage your personal information.
- Member protected health information (PHI) release request form
- Member protected health information (PHI) release request form (Spanish)
- Member request to view claim records form
- Appointment of Representative form
- Member COVID-19 At Home Test Reimbursement form
- Complaint and feedback from: English | Spanish | Arabic | Simplified Chinese | Traditional Chinese | Russian | Somali | Vietnamese
OHP Bridge program benefits
OHP Bridge is a new Oregon Health Plan (OHP) benefit package that covers adults with higher incomes. People who can get OHP Bridge must:
- Be 19 to 65 years old;
- Have an income between 139 percent and 200 percent of the federal poverty level (FPL);
- Have an eligible citizenship or immigration status to qualify; and,
- Not have access to other affordable health insurance.
Expand the section below to learn more about OHP Bridge benefits.
OHP Bridge is almost the same as OHP Plus.
The two benefit packages are almost the same. There are a few things that OHP Bridge does not cover. To learn more about what OHP Bridge does not cover, please see the table below.
| OHP Bridge covers | OHP Bridge does not cover |
|---|---|
|
|
OHP Bridge is free to members. Just like OHP Plus, OHP Bridge is free to members. That means no premiums, no co-payments, no coinsurance, and no deductibles.
OHP members with income changes may be moved to OHP Bridge automatically. If you have OHP now, you don’t have to do anything to get OHP Bridge. If you report a higher income when you renew your OHP, you may be moved to OHP Bridge.
People who do not have OHP right now can apply for OHP Bridge.
Go to Benefits.Oregon.gov to apply. You can also use that link to find information about how to apply in person, get application help, or to get a paper application. To apply over the phone, call the ONE Customer Service Center at 1-800-699-9075 (toll-free, all relay calls are accepted).
